Descriptive or Deceptive Statistics?
A recently published study by the University of Houston sought to analyze trends in chronic pain patients who are either taking opioids alone or together with . [1] To accomplish this goal, users previously registered to Qualtrics, the market research platform, were selectively recruited and promptly approved “[a]fter brief screening for eligibility.” [1] Following statistical analysis, the authors concluded an association between cannabis use during chronic pain-related opioid therapy and “significantly worse mental health and substance use outcomes.” [1] A summary of the survey results are presented below:
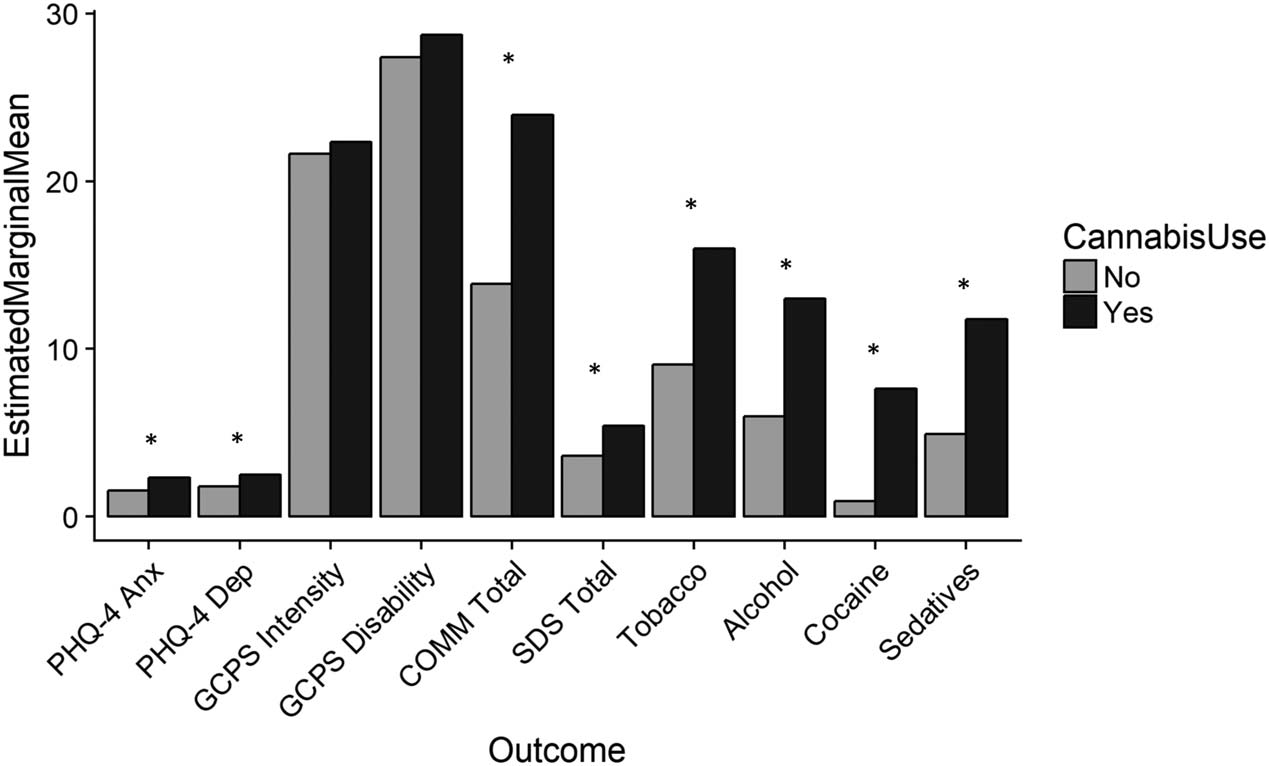
- “PHQ-4 Anx” = Anxiety;
Asterisks (*) indicate a statistically-significant difference in results.
But there are some important reasons why these results are not what they seem.
Survey takers recruited via this process were asked to answer a battery of questions. Among these was an 8-item set of specific inquiries regarding substance use both legal and illicit, which “obtains information from clients about lifetime use of substances, and use of substances and associated problems over the last 3 months.” [2] Specifically, Question 1 searches for endorsement for use over lifetime (“have you ever…”), and Question 2 (Q2) probes for the frequency of said substance use over the past three months (“In the past three months, how often…”).
There are five possible answers to Q2, and it is unfortunate that the authors of this study chose to group everyone who answered anything other than “Never” as one cohort. [1,2] This bulky classification does not separate physician-guided, medically prescribed cannabis use from ‘recreational’ adult use, nor discriminate between chronic pain patients who, on a three-month basis, used cannabis “once or twice” and those who used it “daily or almost daily.” [1]
The same is true for the way this study treated “opioid use.” No attempt was made to differentiate the cohort by type or morphine milligram equivalents of prescription opioids purportedly being used. Finally, the lack of geographic data on the location of those surveyed precludes any comparison across states with varying cannabis laws. These limitations bring into doubt the general associations found. [1]
Further stratifying these relationships, and defining key parameters, is a critical piece that is missing. For example, it remains unclear whether the authors made a good-faith effort to inform potential participants what medications are actually considered a prescription opioid. Outlining a complete list of medications which fall under study design is an important and common practice. [3]
Keep in mind that with only 450 Qualtrics surveyors both qualifying and participating, and only 176 of those claiming any cannabis use, this level of analysis was likely statistically futile due to the small sample size.
When you come right down to it, there’s just a lot of things missing in this study, and their absence is felt. The abstract could just as well read: Out of a cohort of 450 surveyors self-reporting both chronic pain and taking any prescription opioids at unknown dosages and frequencies over a three-month period, just under 40 percent also self-report cannabis use at least once or as much as every day over that same time period. The responses of surveyors to standardized mental health and substance use questionnaires were compared between those who reported any cannabis use and those who did not.
References
- Rogers, A. et al. “Opioid and Cannabis Co-Use among Adults with Chronic Pain: Relations to Substance Misuse, Mental Health, and Pain Experience.” Journal of Addiction Medicine, vol. 13, no. 4, 2019, pp. 287–294 [Times cited = 4, Journal impact factor = 2.406].
- The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) Manual for Use in Primary Care. Prepared by R. Humeniuk et al. Management of Substance Abuse, World Health Organization. Accessed 03 Sept 2019.
- Fiellin, L.Y. et al. “Previous Use of Alcohol, Cigarettes, and Marijuana and Subsequent Abuse of Prescription Opioids in Young Adults.” Journal of Adolescent Health, vol. 52, 2013, pp. 158–163 [Times cited = 71, Journal impact factor = 3.612].
Image Credit: Classic Exhibits