Humans have been drawn to hallucinogenic compounds for thousands of years. Paintings of suspected psychedelic mushrooms have been found in North African and European caves which have been dated as far back as 9,000 years ago. In ancient times, psychedelic experiences served as religious instruments and were also used in healing rituals. Despite being illegal in most parts of the world, psychedelics are still in use today.
For many psychedelics users, ego dissolution aka ego death is the highest reward that one can achieve from a good trip. However, most users acknowledge how varied and subjective experiences from each trip can be. While one experience can be mystical and revealing, a different one can trigger intense terror and panic. That has been acceptable, but is now posing a challenge as psychedelics therapy is becoming mainstream.
A series of clinical studies on psychedelics that have been conducted recently have revealed the potential of psychedelics in treating psychiatric conditions. As scientists endeavor to bring hallucinogenic compounds into mainstream medical practice, the variability in individual experiences poses a challenge.
One clinical trial examined 13 patients who were started on psilocybin-assisted psychotherapy for treatment-resistant depression. [1] (Psilocybin is the active ingredient in hallucinogenic mushrooms). The study showed that 71% of the participants experienced significant therapeutic benefits after two doses of psilocybin treatment.
Psychedelics and Neurotransmitters
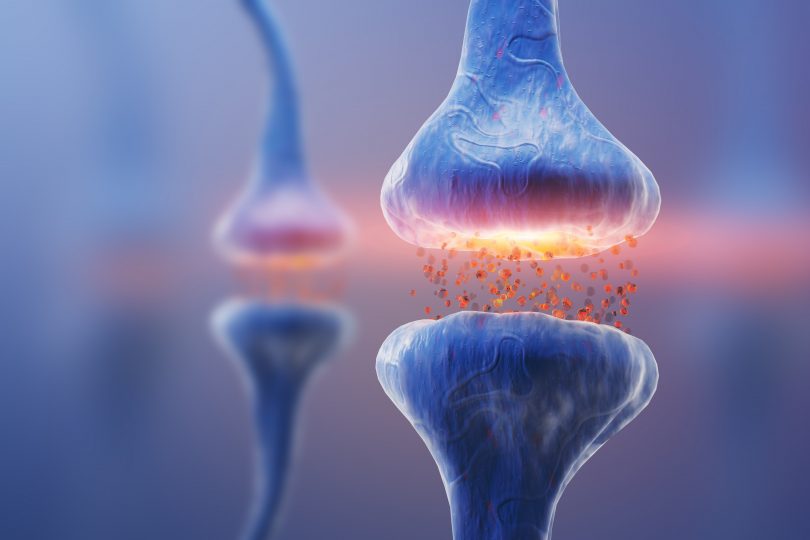
A group of psychedelics researchers conducted a review in 2021 to establish the relationship between psychedelics, neurotransmitters, and subjective experiences. [2] The “classical psychedelic neurotransmitter” is considered to be the 5-HT2A receptor. This neurotransmitter is targeted by classical psychedelics including lysergic acid diethylamide (LSD), psilocybin, mescaline, and N,N-dimethyltryptamine (DMT).
They explored 6,850 testimonials involving 27 drugs which were observed through 40 prisms of neurotransmitter subtypes. The researchers then mapped 3D coordinates of the brain using invasive tissue probes based on their findings. This technique delineated how subjective psychedelic experiences (fractal distortion of visual perception and ego death) are linked to the anatomical distribution of receptor subtypes.
From the review, the researchers were able to identify neurotransmitter receptor subtypes that are involved in psychedelic experiences. The most dominant receptors involved included 5-HT2A, dopamine D2 (involved in locomotion, attention, sleep, memory, learning), kappa opioid receptor (involved in pain, consciousness, mood, addiction, and N-methyl-d-aspartate (involved in mood, memory, excitotoxicity) receptors, which are primarily anchored in both the deep cortex (causing ego dissolution) as well as the shallow (visual) cortex. The researchers also found that subjective experiences may be triggered by selective affinity for the 5HT2A receptor. [2]
As much as this is a preliminary study, it preempts the need for future clinical trials that will unlock the far-reaching potential of psychedelics-assisted psychotherapy.
Image Source
https://freesvg.org/psychedelics
References
[1] Davis AK, Barrett FS, May DG, et al. Effects of psilocybin-assisted therapy on major depressive disorder: A randomized clinical trial [published correction appears in JAMA Psychiatry. 2021 Feb 10;]. JAMA Psychiatry. 2021;78(5):481-489. [journal impact factor = 21.6; times cited = 154][2] Ballentine G, Friedman SF, & Bzdok D. Trips and neurotransmitters: Discovering principled patterns across 6,850 hallucinogenic experiences. bioRxiv. 2021. [journal impact factor = N/A; times cited = 2]